Injuries Treated by PRP Therapy Include:
- Chronic Sports Injuries (ex. Tennis Elbow, Achilles Tendonitis, and Runner’s Knee)
- Degenerative Joint & Disc Disease
- Chronic Sprains and Strains
- Cervical, Thoracic, and Lumbar Spine Strains
- Traumatic Brain injuries
- Arthritic Joints
- Shoulder Pain, Hip Pain, and Knee Pain
- Ligament Laxity or Tears
- Tendon and Ligament Injuries
- Carpal Tunnel Syndrome
The PRP (platelet rich plasma aka “bioactive whole plasma”) injection treatments used by Dr. John Hughes (and associated osteopathic practitioners) are unique to Aspen Integrative Medicine and unlike the PRP injections provided by an orthopedic clinic. Such clinics routinely treat patients with one injection of a small amount of PRP with the intended goal of calming inflammation (as with cortisone). Many patients treated by these orthopedic clinics report limited success from this inadequate use of PRP.
PRP Versus Prolotherapy: A Supercharged Option
“Prolotherapy is like planting seeds in a garden;
PRP therapy is planting seeds with fertilizer.”
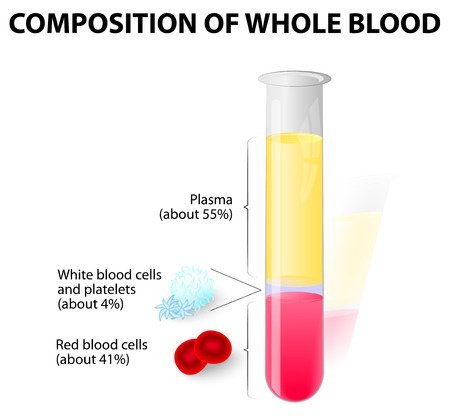
Platelet rich plasma (PRP) therapy, like prolotherapy, is a method of injection designed to stimulate healing. “Platelet rich plasma” is defined as “autologous blood with concentrations of platelets above baseline levels,” “which contains at least seven growth factors.” Cell ratios in normal blood contain only 6% platelets, however, in PRP, there is a concentration of 94% platelets. Platelets contain a number of proteins, cytokines and other bioactive factors that initiate and regulate basic aspects of natural wound healing. Circulating platelets secrete growth factors, such as platelet-derived growth factor (stimulates cell replication, angiogenesis), vascular endothelial growth factor (angiogenesis), fibroblast growth factor (proliferation of myoblasts and angiogenesis), and insulin-like growth factor-1 (mediates growth and repair of skeletal muscle), among others. Enhanced healing is possible when platelet concentration is increased with PRP. Activated platelets “signal” to distant repair cells, including adult stem cells, to come to the injury site. Increasing the volume of platelets accordingly increases the subsequent influx of repair and stem cells. Because the concentrated platelets are suspended in a small volume of plasma, the three plasma proteins fibrin, fibronectin, and vitronectin contribute to a repair matrix. You could compare dextrose prolotherapy and PRP this way: prolotherapy is like planting seeds in a garden; PRP therapy is planting seeds with fertilizer.
A Powerful Form of Regenerative Injection Therapy
The concentrated platelets found in PRP include growth factors among the huge reservoirs of bioactive proteins that are vital to initiate and accelerate tissue repair and regeneration. These bioactive proteins can help increase stem cell production to stimulate connective tissue healing, bone regeneration and repair, development of new blood vessels, and wound healing.
How Does PRP Therapy Work?
Dr Hughes (and associated practitioners at Aspen Integrative Medicine) employ “PRP” in the following ways.
1) “PRP” utilized by Dr. Hughes includes not only the platelet rich plasma but all of the plasma collected from a blood draw including the platelet poor plasma (PPP) which actually contains many more stem cells than the PRP.
2) Dr. Hughes activates this whole plasma with ozone as well as vitamin C, magnesium, and dextrose and a green laser light. The resulting “bioactive whole plasma” is super oxygenated and more metabolically robust than the typical PRP injected by most other clinics.
3) Before injecting this bioactive plasma, Dr. Hughes performs an osteopathic manual exam to identify the tissues that are most injured around the neck, back, shoulder, elbow, sacrum, hip, knee, ankle, or foot. Dr. Hughes will then review ultrasound or MRI imaging studies to determine which tissues might have tendinosis, fibrotic scar tissue, degeneration, sprains, or strains.
4) Unlike most orthopedic clinics, Dr. Hughes often pinpoints 4-7 areas to inject in shoulders, elbows, knees, wrists, hip, and ankles and 8-10 areas of injection for the neck, back, pelvis, sacrum, or hip. Dr. Hughes uses so many more bioactive, whole plasma injections than most orthopedic clinics because he understands that bioactive plasma can heal the damaged musculoskeletal tissues rather than just calm the inflammation associated with injury.
5) In addition to injecting damaged joints, ligaments, tendons, or muscles, Dr. Hughes actually performs curettage and tenolysis of these tissues as necessary. In other words, Dr. Hughes will carefully scrape away (using a small needle) calcified tissue debris in the joints (such as with bone spurs or chondrosis), tendons (as calcific tendinosis) or ligaments (as fibrosis) before injecting bioactive plasma.
6) Also, all injection patients are carefully supported in a holistic nutritional sense with IV nutrition (including Vit C, b vitamins, and minerals) provided before the injections and specialized oral nutrients and guidance provided for weeks after the injection procedures. Patients are also directed to appropriate PT or manual therapy as well as shockwave therapies post-treatment by local practitioners such as Dr. Eric Haynie.
7) Finally, all patients have the option of using pain medications (such as Trammadol or Percocet) as needed post-injection and a sedative (such as Valium) and local anesthetic (Ropivacaine) before receiving the precisely guided bioactive, whole plasma or peripheral blood stem cells injections by Dr. Hughes or associated osteopathic practitioners.
How to Heal from PRP
- Nutritional status is really important. Patients who regularly consume inflammatory foods such as dairy products (especially cow’s milk cheese), wheat (high gluten), refined sugars, and soy products are most at risk for systemic inflammation that can localize to the knee, hip, or other joints that are regularly used. It is important to minimize these foods before and at least 3 weeks after injections of PRP (as bioactive plasma) or PBSCs (Peripheral Blood Stem Cells). *Note: The proteins in dairy (casein, whey), wheat (gluten), and soy commonly are poorly digestible and thus get across the gut membrane causing the body to create an immune response because they are viewed by the immune system as a foreign body or invader. This immune system response creates inflammation (calcifications-in the case of dairy) in commonly used joints.
- In addition to limiting dairy, wheat, and soy, it is important for patients to avoid calcium supplements that are made with calcium carbonate (such as Tums, Ostcal). Dr. Hughes regularly recommends a supplement called Super Phosphozyme (Biotics) to improve the calcium/phosphorus ratio in the body for patients with significant calcinosis or fibrotic lesions in their joints, tendons, or ligaments. Patients regularly are prescribed 2 pills 2x/day of Super Phosphozyme for one month after the injection and curettage procedure of PRP (as bioactive plasma) or PBSCs (Peripheral Blood Stem Cells).
- Patients with systemic inflammation may also consider proteolytic enzymes that can be taken on an empty stomach. Usual dosing is 3-4 pills 2x/day on empty stomach (2 hours after a meal) or as needed. Common proteolytic supplements include Vitalzym, Doctor’s Best, Serropeptase, or Wobenzyme. These supplements, of note, may be taken before the injection of PRP (as bioactive plasma) or PBSCs (Peripheral Blood Stem Cells) but should not be taken for at least 3 weeks post-procedure. Other natural antiinflammatories such as turmeric or fish oil as well as NSAIDs including aspirin, naproxen, or ibuprofen. Blood thinners such as vitamin E or warfarin, or heparin based medications should also be avoided.
- Finally, allowing time for tissue regeneration is really important post-injection. Patients of Aspen Integrative Medicine are advised to avoid much activity the first 2-4 days after getting injected and then slowly increase their activity level by 20 percent per week for the next 4 weeks. For joint recovery, Dr. Hughes regularly recommends 2 to 4 pills of Elk Antler (from High Wire Ranch) supplements and sometimes hyaluronic acid or glucosamine.
- Getting PT, acupuncture, or massage therapy along with shockwave treatments can also be very helpful post-injection. Dr. Eric Haynie of Aspen is a specialist in using shockwave treatments to bring blood flow and restore damaged or fibrosed tissues and accelerate the healing process.
I’m a disabled Vietnam Veteran and I have full medical care at the VA Hospital but they are not able to do what Dr. Hughes has been able to accomplish. He’s been able to reduce my pain medication by seventy five percent and the shots that he has given me in my lower back, due to degenerative disc disease, have increased my way of life.*
Frequently Asked Questions
Are PRP Injections a Good Alternative to Cortisone Shots?
Studies have shown that cortisone injections actually weaken tissue and serve to further degenerate damaged cartilage. Cortisone shots may provide temporary relief and decrease inflammation, but generally do not provide long-term healing. PRP therapy acts to heal and strengthen tendons and ligaments, and, in some cases, thickens the tissue up to 40%.*
*Results may vary; no guarantee of specific results
How Many PRP Injections Are Needed? How Often?
While responses to treatment vary, most people will require 1 to 3 sets of PRP injections at our Colorado clinics. Each set of PRP treatments is spaced 2 to 4 weeks apart.
What Is Recommended During and After PRP Treatment?
You are restricted from the use of non-steroidal anti-inflammatory medications (NSAIDs) one week prior to the PRP procedure and throughout the course of treatments. Initially, the procedure may cause some localized soreness and discomfort. Patients rarely require some extra-strength Tylenol to help with the pain. Ice and heat may be applied to the area as needed.
What Is the Recovery Time Following PRP Injections?
Is PRP Therapy Covered By Insurance?
Typically PRP therapy is not covered by insurance. Also known as proliferation therapy, it is considered experimental and investigational for all indications because there is inadequate evidence of its effectiveness with limited clinical trials. Your insurance may, however, cover the cost of the initial consultation or ultrasound imaging if it is needed for guidance.
How Much Does PRP Therapy Cost?
The cost of PRP therapy depends on the treated body area, complexity, and number of injections needed. Typical PRP procedures start at $2,500 or more on average.